Cryptosporidiosis in Angora Goats
By Dr Mackie Hobson BSc(Agric),BVSc
Tuesday, 20th September 2022Cryptosporidiosis referred to as ‘Crypto’ has been a major problem in calves and lambs under intensive conditions in South Africa since 2013.
The first cases of Cryptosporidiosis in Angora goat kids were recorded in Australia in 1981.
Before 1980 cryptosporidiosis was considered rare throughout the world and was first reported to cause diarrhoea in cattle in 1971. The first cases in humans was discovered in 1976. The disease has progressed to become a major problem internationally and has developed to a point where 38% of the reported neonatal calf scours in the UK is due to Cryptosporidiosis.
The current extent of the distribution of Cryptosporidium throughout South Africa is unknown, but most provinces have had outbreaks.
The first explosive outbreaks in sheep occurred in the Eastern Free State in 2013. In Angora goats, cases were first detected along the Fish River and associated irrigated pastures starting in 2019.
In the extensive areas of the Karoo, the first incidental detection of Cryptosporidium was in 2013 in the Graaff-Reinet area; however, there were no reported cases of Crypto until after 2021 when:
- Sheep introduced from the Fish River irrigation region resulted in a confirmed outbreak in lambs.
- Further positive case was detected in young Angora goats (year old) where diarrhoea and a few deaths occurred in the Rietbron district, Coccidiosis and crypto were detected on histopathology.
- Since then further outbreaks (not associated with river contamination but with the movement of animals) have been diagnosed in Graaff-Reinet and Willowmore.
- Screening tests using Modified Ziehl-Neelsen (mZN) Microscopic staining of faecal samples has suggested that crypto may be present on many more farms that have not had clinical outbreaks of Crypto. See https://www.angoras.co.za/article/crypto-screening-for-sub-clinical-carriers#399

Cryptosporidium parvum, a protozoa which is about a 10th of the size of a Coccidia oocyte, causes diarrhoea in young and immunocompromised animals and is usually associated with explosive outbreaks.
It can be transmitted from man to animals (Zooanthroponosis) and animals to man (Zoonosis). The initial outbreaks in South Africa were likely from human sewerage effluent entering our river and water systems and ending up on irrigated pastures or in livestock drinking water.
In South Africa, the initial explosive outbreaks resulted in losses of 10-50% of lambs on affected farms in the Eastern Free State. During the following years, the outbreaks tended to occur more during the tail end of lambing as immunity built up and the transfer of antibodies occurred through the colostrum. However, explosive outbreaks have recurred a few years after the initial outbreak on some farms.
What age of kids are affected?
Infection usually occurs in kids 1-4 weeks old (5-14 days but up to 3 months). Outbreaks are likely to be seen in intensive conditions such as lambing pens, ’kraaling’ at night, irrigated pastures and kidding in small camps.
How can Angora kids be infected?
The infection is via contaminated food or water or directly between shedding individuals via the faecal-oral route. The oocytes shed in the faeces are very resistant in the environment and may survive for a year/s, and they can survive temperatures ranging from -20 to 60°C. These oocytes can spread via subclinical carriers, waterways, fomites, wildlife, flies, mechanical vectors and humans.
The movement of subclinical carriers (goats and sheep) between farms is of concern within the mohair industry. These carriers can introduce oocytes that can then be picked up by the kids/lambs during the following kidding season and result in an outbreak, as has already occurred in the Graaff-Reinet, Rietbron and Willowmore districts.
It is thought that as few as 10 oocytes can cause disease in calves and 1 oocyst in lambs/kids. Billions of oocytes can potentially be shed by an acutely infected kid (>100 000 per gram faeces).
The life cycle of Crypto
Oocytes are taken orally and contain 4 sporozoites which are released after ingestion. These sporozoites invade the intestine cells, going through several life stages to ultimately produce oocytes. These oocytes are thick and thin-walled. The thin wall oocytes rupture, resulting in autoinfection. The thick-walled oocytes pass out through the faeces to contaminate the environment.
The life cycle is rapid and can be as short as 3-4 days.
Crypto lives for about 5 weeks in the intestine and can survive for years in the environment as thick-walled oocytes.
What happens to the intestinal wall after infection?
The infection leads to cell destruction of the intestinal wall resulting in atrophy and fusion of intestinal villi (the finger-like projections from the intestinal wall responsible for nutrient absorption). The destruction of cells leaves them vulnerable to invasion by intestinal bacteria and viruses.
Clinical signs:
The incubation period is 2-7 days but can be as long as 10 days. Clinical signs usually last 2 weeks, and animals can relapse a week or two after recovery. Recovery may take up to 30 days.
Kids in the first two weeks of life are most affected, but up to 3 months can show clinical signs. Older kids are often asymptomatic but deaths have been diagnosed in young Angora goats (1 year) when both Crypto and Cocci were detected.
-
Except when occurring in very young kids, the infection is not often detected or causes mild diarrhoea. It has however been detected on Post Mortem in young goats (1 year old) where together with Coccidiosis had caused deaths.
- The rectal temperature is usually 40 °C.
- Reduced appetite, lethargy at the start, followed by diarrhoea.
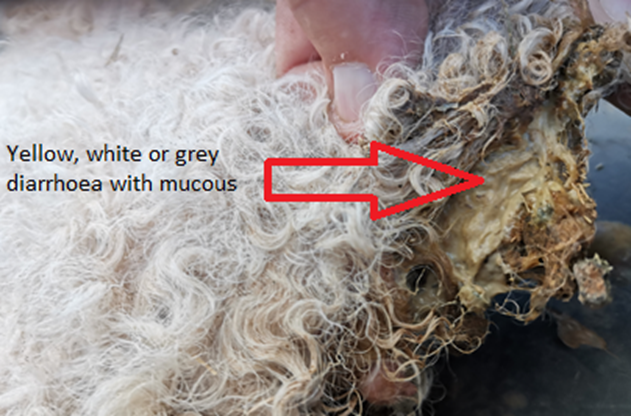
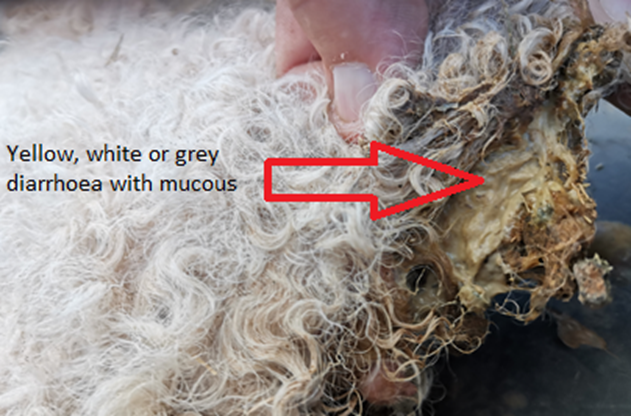
- A profuse yellow, white or grey diarrhoea with mucous can occur in kids.
- Kids will be anorexic and depressed.
- Loss of body weight
- The kid may strain to defecate and show abdominal pain.
- Stiffness, hyperpnoea (rapid breathing), slow gait and depression
- Dehydration and death may follow.
The symptoms in those that survive usually last 7-15 days.
What is seen on a Post Mortem examination?
- Dehydrated young kids
- Intestine gas-filled and contains yellow watery fluid
- Lesions are found in the ileum, caecum and colon.
- Inflamed intestines

Ideally, the farmer does not want to be faced with the problem of Cryptosporidiosis so BIOSECURITY of the farm is critical.
Ensure you have an owner’s declaration signed by the owner’s vet or agent that cryptosporidiosis has not been diagnosed on the farm when purchasing goats.
The protocol on your farm must not only be for animals being introduced but include vehicles and people entering your farm. You don’t want visitors parking near your animal handling facilities or in areas where your stock may graze!
As adult goats can carry cryptosporidiosis, the producer may only see the first signs of crypto when kidding the following year. So after quarantine, still keep introduced goat ewes on their own away from your breeding flock until after kidding. Be aware of your water drainage systems.
No biosecurity protocol is fool proof, but it is about reducing your risk.
Buy your goats from farms you know and trust that are also adapted to your environment and production system type and request a vendor health declaration.
For more information on detecting sub-clinical carriers, see:
https://www.angoras.co.za/article/crypto-screening-for-sub-clinical-carriers#399
WHAT TO DO IN AN OUTBREAK?
Make sure you have a positive diagnosis from your vet.
Biosecurity Protocols
- Isolate and quarantine sick kids with their ewes (move the healthy ewes/kids out of the camp/pen and leave the sick in)
- Move the healthy ewes out of the infected camp - use a footbath with Chlorine dioxide and clean/spray the udders (see below disinfectant section)
- Ensure the healthy ewes and kids are divided into the smallest groups that you can. This will limit the number of infections as much as possible. (1 infecting 25 or 50 rather than 500)
- Keep the last 20% of ewes to kid in a separate camp as contamination of the environment tends to build up from the older shedding kids.
- Watch out for mechanical transmission (clothing, people, dogs, vehicle and equipment movement).
- Check drainage areas from contaminated areas
- Avoid moist areas, leaking troughs.
- Ensure feed and water troughs are at a height where faecal contamination cannot occur.
Treatment
Remember it is a zoonosis (humans can get it) so use PPE and hygiene protocols.
A number of protocols have shown to be of benefit as outlined in points A to G below.
The following treatments have been shown to be of benefit in treating Crypto.
A: Treat the Crypto with one of A1, A2 or A3
A1: Parofor (Licensed)
A2: Halcocur (Off label)
A3: AQUAVi2000-500 (Off label)
 |
 |
|
A3) AQUAVi2000-500 (Ready to Use- RTU)
Used off label
RTU solution of 2000ppm Chlorine Dioxide stock can be purchased.
Make up to 300ppm solution by
- 150ml of stock solution (2000ppm) + 850ml water (makes up a litre of 300ppm ready to treat)
- Dose each kid with 20ml of diluted solution (300ppm) a day
|
 |
|
C) Electrolyte mixtures:
- Ensure sick kids are rehydrated. Administer 100 ml of an electrolyte mixture up to 3 times a day if possible
(The equivalent of 10-20% of body mass a day).
- Administer electrolytes prior to the Halocur treatment
Examples of electrolytes: Repensol, Diakur, Lectade
|
|
D) Mineral Vitamin supplements:
- Vit E, Selenium: Inject on day 2 after birth (There are a number of products available
https://www.angoras.co.za/article/mineral-and-vitamin-options
- Immunovite (MSD) Use 0.75 - 1 ml undiluted product per kg body mass for optimum support.
Bacillus amyloliquefaciens acts as a probiotic with fulvic acid to provide functioning support to the gastrointestinal tract
with healing properties.
It contains vitamins and certain trace elements (It does not contain Selenium or Vitamin E)
|
|
E) Treat the Pain/Inflammation:
Most kids will have a fever (>40C) and have abdominal pain.
- Inject 0.25ml/10kg Meloxicam (20mg/ml) under the skin -The effect lasts for 3 days.
|
|
F) Probiotics
Examples:
- EM1 (Effective Microbes) kids 2 ml after birth, can add to water 1:1000 daily.
- Immunovite (as per Mineral Vitamin above in section c)
Other examples include Protexin, Biorem. |
|
G) Antibiotics
If indicated (secondary infections in those with clinical signs).
|
|
Other treatments include:
- Nekka-Rich (Four Lakes) This is activated charcoal and wood vinegar and has shown efficacy
in reducing or eliminating Cryptosporidium parvumin calves.
Treatment Dose: 5g per kid (20g for calf) twice a day for 4 days.
Also, give electrolytes at the same time of treatment.
- It has also been reported that Activated charcoal (Dosed or tubed at 2g/kg body weight) and Garlic is beneficial.
Many more products will become available on the market.
|
REDUCE THE IMPACT OF CRYPTO BEFORE the ewes start kidding on a Crypto positive farm?
- Add ‘Deccox’(Decoquinate) Zoeitis to feed of ewes 4 weeks before kidding and continue to 2+ week after kidding.
- Deccox is not licenced for crypto, but it has been demonstrated in trials that if ewes/cows are given Decoquinate in feed 4 weeks before and 1 week after kidding at 1.25mg/kg a day, it prevents the appearance of crypto.
- This was also shown in cows (4 weeks before to 1 week after calving) at 1.25mg/kg prevented crypto (Havant, Cantaloube) over a 7 year trial period.
- This finding was repeated in trials by Bremmer and Richard in Scotland with the same results.
- Infected kids treated at 2.5mg/kg reduced the severity of the crypto and reduced shedding. This was also demonstrated in the reduction in calves when treated from day 3 to 17.
- However, Lallemand et al 2006, Moore et al 2003 said Decoquinate was ineffective against crypto.
- Vaccinate the ewes 4-6 weeks before kidding (Multi-clostridium Vaccine) Antibodies are carried over in colostrum
- Give Mineral and Vitamin supplements 4-6 weeks before kidding. Carried over in colostrum to the kid. See options on website https://www.angoras.co.za/article/mineral-and-vitamin-options#360
- Ensure good nutrition for 4 weeks before kidding and 2 weeks into kidding. This ensures good and plentiful colostrum production. With added Deccox!
- Separate the pregnant ewes into the smallest groups possible. This reduces the risk when kidding as 1 sick kid infects 50 instead of 500 (or less if possible).
- Keep the ewes that will kid last separate from earlier kidding ewes. This reduces the build-up of oocytes in the environment to infect the late-born kids.
There is no vaccination against Crypto. The manufacturer of a vaccine in Europe was attempted but was ineffective.
What can be done to reduce environmental Crypto (intensive systems such as kidding pens?)
Disinfect kidding areas and equipment with one of the following—treatment of water sources.
- Chlorine dioxide
Trials have shown Chlorine dioxide can inactivate cryptosporidium oocytes. (5mg/l) (50ppm)
50ppm safe both as a disinfectant to treat the environment and in drinking water. *
50ppm 1-2 minutes contact time **
Products include:
- Nanotech SA
- AQUAVi2000-500
- OxyFect® 8504
- OxyAzur® Duo Chlorine Dioxide Detergent-disinfectant - Tristel
- Biox 5000 Chlorine Dioxide Disinfectant - Xie Import & Export
- Xzioxa Mix Chlorine Dioxide Disinfectant - Taiaha SA KZN
- Dutrion Chlorine Dioxide Disinfectant - Green Technologies SA
- Calgonit CD-K System Chlorine Dioxide Disinfectant - ImproChem GP
- Surface Gene Chlorine Dioxide Disinfectant - Process Catalysts CC
- Vital Oxide Chlorine Dioxide Disinfectant - Protectapak CC
- Aqquon 20 Chlorine Dioxide Disinfectant - WR Petroleum Logistics
- Xziox Mixed Chlorine Dioxide Disinfectant - Mpumamanzi Group
- Dutrion Chlorine Dioxide Disinfectant
- Vital Oxide Chlorine Dioxide Disinfectant
- Kenocox
Effective against Cryptosporidium. Spray a 2% solution, rinse feeding and drinking troughs. For Crypto dilute 1:50 (contact time 2 hours)
4% (1:25) also eliminates Coccidiosis
- Neopredisan
Neopredisan 135-1 (Bupo Animal Health)
Proved effective against crypto at 3% for 1 hr (Mix 30ml to litre water)
Neopredisan is also effective against coccidiosis.
- Hydrogen peroxide
3% solution inactivates Cryptosporidium in 40 minutes and eradicates in 30 minutes
Don’t use water containing Chlorine (municipal water) as antagonists.
- Afrisan Peroxsil Ag+ (SABS approved)
- 10% Formalin(irritates mucous membranes of nasal passages and eyes) Not recommended
2 hours later, after disinfecting, overwhelm the area with good bacteria
- Expanded EM) 1:50 if using small ‘lambing pens’. Not practical in larger areas.
- EM Technolgy application (MZP), Developed in Japan. EMViro Environmental application for Pens/barns 1:50 daily for a week then 1:200 weekly. Dams/effluent ponds: 1:1000 by dam volume then 1:5000 by dam volume
Boiling, steam, pasteurisation and industrial UV light are also effective in killing crypto
Bleach, chlorine, alcohols, phenols, Quaternary Ammonium products and iodine are NOT effective.
Ploughing up land contaminated with crypto may bury the oocytes and reduce oral intake.
During an outbreak, attempt frequent removal of faeces if possible.
Diagnosis: Post Mortem Tests and Sampling.
A presumptive diagnosis can be made on history and clinical signs as well as a positive ‘Rapid Test’, but a definitive diagnosis must be made by:
- Histopathology: 2 sample pieces of the duodenum, jejenum, and proximal colon should be taken, placed in 10% formalin and sent to the laboratory.
- A culture sample helps determine if other pathogens are present (E, Coli, Salmonella or Clostridia). Important in calves for Rota, Salmonella, E.Coli.
- Rapid Test Antigen swabs are taken from the ileo-caecal junction. This allows a quick on-site presumptive diagnosis. Take the sample from the ileum side of the junction. The Rapid Tests (Antigen detection) include:
- Zoetis WITNESS Bovid-5 Test
- Afrivet Rapid Test kit Bovid-5
- Pet-X Rapid Test kit

- Modified Ziehl-Neelsen (mZN) Microscopic staining of faecal samples. Faecal samples are sent a ‘cold chain’ to the laboratory.
THE RAPID Antigen Tests as a SCREENING TEST on rectal or faecal samples from suspected SUBCLINICAL CARRIERS IS NOT EFFECTIVE.
For work done on detecting SUBCLINICAL CARRIERS see https://www.angoras.co.za/article/cryptosporidiosis-in-angora-goats
Collection and storage of samples:
Faecal samples for Cryptosporidium should be tested as soon as possible. Alternatively, samples can be frozen or preserved with 10% formalin if testing can only be done at a later date. However, if PCR-based techniques are to be used, formalin can reduce the sensitivity of PCR. Freezing is also not advised if PCR is to be done (Vetdiagnostix)
Since the shedding of cysts may be sporadic, at least three consecutive samples should be collected or possibly taking a pooled sample from 5 + individuals to account for sporadic shedding. Take rectal faecal samples.
INFORMATION OF INTEREST:
The development of immunity
Cryptosporidiosis in ruminants is a neonatal disease, and adults are seldom affected. This suggests immunity plays a major role in reducing the impact of the disease. Both acquired immunity and host age determine the susceptibility to and severity of infection.
The following years after an outbreak, the transfer of antibodies in the colostrum is essential. It reduces the impact of Crypto with usually only the tail end of kidding/lambing a problem due to the increased environmental challenge.
Angora goats have a poorer innate/acquired immunity than other goats up to nearly a year of age. See article on the immunity of the Angora goat https://www.angoras.co.za/article/immunity-in-angora-goats
No successful vaccine has been developed.
What is the incidence of Cryptosporidium in wildlife?
Surveys in the Kruger National Park tested 445 samples.
Elephant (25.8%), buffalo (5.5%) and impala (4.3%) tested positive.
There were significantly more positives from animals adjacent to the western boundary (human, domestic animal transmission?).
Cryptosporidium in humans
What are the symptoms in humans?
The diarrhoea is profuse and watery; it may contain mucus but rarely blood. It is often associated with weight loss. Other less common clinical features include abdominal pain, nausea and vomiting, and a low-grade fever
Human outbreaks and prevalence:
- 1987, cryptosporidiosis was associated with 13,000 cases of gastroenteritis in Georgia
- In 1988 and 1989, two Cryptosporidium-related waterborne outbreaks were reported in Ayshire, Scotland, and Oxfordshire-Swindon,
- Cryptosporidiosis was reported in 1993 in Milwaukee, Wisconsin, the USA, where an estimated 403,000 people were infected due to faulty filtration of the water.
- Prevalence rates in Europe were reported to be 1 to 2%. North America prevalence of 0.6 to 4.3% is lower than those reported in surveys from Asia, Australia, Africa, and Central and South America, ranging from 3 to 20%.
- Prevalence was highest in children less than 2 years of age, and infections were often seasonal, with a higher prevalence during warmer, wetter months.
- Sero-prevalence rates in Europe and North America are usually between 25- 35% compared to 64% in South America.
The different tests for detecting Crypto
- Direct microscopic examination
As the cysts of Cryptosporidium are tiny, a staining procedure is required to identify them. Conventional methods of stool examination (i.e., routine "stool for ova and parasites" testing) are unreliable.
A number of different staining techniques have been developed.
- Ziehl-Neelsen (ZN) is an Acid-fast procedure -staining is a bacteriological stain used to identify acid-fast organisms. Acid Fast positivecells are stained pink/red, and Acid Fast negative cells are stained the light blue colour of methylene blue.
- Modified Ziehl-Neelsen (mZN) -with this method, the dyeing time is shortened, and heating is not required.
- Auramine Phenol (AP) The parasites appear greenish-yellow against a dark background. The method is more rapid and sensitive than ZN technique.
- Immunoflourescence Microscopy (IFM) is a widely used example of immunostaining and is a form of immunohistochemistry. Specific antibodies bind to the protein of interest. Fluorescent dyes are coupled to these immune complexes in order to visualize the protein of interest using microscopy. IF microscopy can be used in several microscope designs for the analysis of immunofluorescence samples.
- Immunology:
Detect soluble protozoan antigens in faecal samples, thus removing the need for microscopic examination.
- Enzyme immunoassay (EIA) and enzyme-linked immunosorbent assay (ELISA) technologies have been used to develop commercial products for the detection of Cryptosporidium
EIA, ELISA has the advantage of good specificity, and a large number of samples can be processed in a short time.
- Immunochromatographic lateral-flow (IC) or (ICLF) 'dipstick' tests have also been developed for antigen detection in stool samples. These tests are sensitive and specific, easy to use and provide a result in 10 minutes.
Immunochromatography is a test format that uses tagged particles as a colour signal rather than an enzyme-catalyzed colour change reaction as in ELISA. The test uses biologics and tagged microparticles coated with specific Crypto antibodies.
These ICLF tests are the Rapid tests used in the field.
- Molecular biology
PCR or real-time PCR (RT-PCR) is a molecular biology-based diagnostic detection method developed to target specific sequences in the protozoan genome. These methods offer highly specific and sensitive assays but are expensive and time-consuming.
- PCR is the GOLD STANDARD test- are more sensitive with the detection range from 1 to 106oocysts, are relatively rapid, and have the major advantage of speciation, which is very important from an epidemiological point. This comes with costs and time disadvantages.
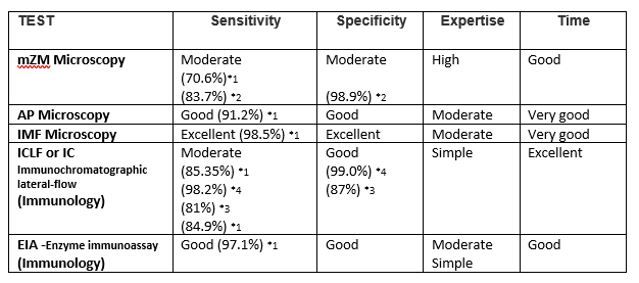
Comparing the SENSITIVITY and SPECIFICITY of the different Tests
What are sensitivity and specificity?
Sensitivity is the ability of a test to correctly identify the animals with crypto (True Positive).
Specificity is the ability of a test to correctly identify animals without crypto (True negative).
PCR is considered the gold standard to test for the presence of Cryptosporidium.
COMPARING the different tests in the table below:
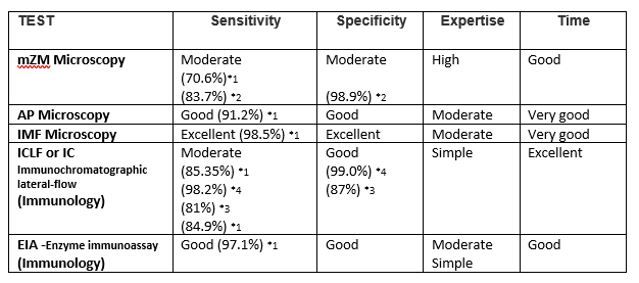
HOWEVER, these sensitivity and specificity are tests on samples from cases showing clinical signs.
The ability of these tests to pick up SUBCLINICAL CARRIERS (i.e. goats that are not showing any clinical signs but are shedding low numbers of Cryptosporidium oocytes)?
Microscopic staining techniques, mZN (Dr Jacob Stroebel-Western Cape laboratory), were able to detect carriers with less than 1 per 400X field on average. PCR (Vetdiagnostix) and ICLF tests could not detect healthy carriers.
For information on detecting sub-clinical carriers, see
https://www.angoras.co.za/article/crypto-screening-for-sub-clinical-carriers#399
Dr Mackie Hobson, BSc (Agric) BVSc
Mohair SA, SAMGA Veterinarian
With special thanks to Dr Liezel Wasserman from the Clocolan Veterinary Clinic for sharing her expertise and experience working with Cryptosporidiosis
References
- Dr Liezel Wasserman (Clocolan Veterinary Clinic)
- Dr James Hill (Vetdiagnostix)
- Dr Jacob Stroebel (Western Cape Laboratories)
- *Efficacy and Safety Evaluation of a Chlorine Dioxide Solution by Jui-Wen Ma 1,2,Bin-Syuan Huang Chu-Wei Hsu ,Chun-Wei Peng ,Ming-Long Cheng ,Jung-Yie Kao ,Tzong-Der Way ,Hao-Chang Yin and Shan-Shue Wang
- ** Bovine veterinarian Jan 2015 John Maday
- Efficacy of Two Peroxygen-Based Disinfectants for Inactivation of Cryptosporidium parvum Oocysts. Joaquin Quilez,* Caridad Sanchez-Acedo, Catalina Avendan˜o, Emilio del Cacho,and Fernando Lopez-Bernad
- Dr Marijke Henton
- The prevelance of Cryptosporidium in wild animals in the Kruger National Park. Nada Abu Samra, Ferran Jori, Amidou Samie, Peter Thompsom
- Aust Vet J. 1981 Aug 57(8):386-8.Intestinal cryptosporidiosis in a kid goat.
- Genetic Characterisation of Cryptosporidium spp in diarrhoeic Children from four provinces in South Africa, Abu Samra, P. Thompson, F,Jori, J Frean, B.Poonsamy, D du Plessis, B Mogoye,L. Xiao
- Mason RW, Hartley WJ, Tilt L.
- MSD Veterinary manual
- Infectious Diseases of Livestock Coetzer, Thomson, Tustin
- Aust Vet J. 1981 Aug;57(8):386-8. Intestinal cryptosporidiosis in a kid goat. Mason RW, Hartley WJ).
- Cryptosporidiosis WILLIAM L. CURRENT' AND LYNNE S. GARCIA
- Cryptosporidiosis control in ruminats: Franck Foulon,
- Veterinary Investigation Surveillance Report (VIDA, 2012))
- Cryptosporidiosis in Cattle,The Moredun Foundation,Beth Wells BSc, PhD,Sarah Thomson
- Laboratory diagnosis of cryptosporidiosis Sumeeta Khurana and Preeti Chaudhary
- Cryptosporidium/Giardia Detection and Identification Methods in Water Treatment, Clinical, and Food Applications, Rapid Microbiology
- *2 Comparison of PCR and Microscopy for Detection of Cryptosporidium parvum in Human Fecal Specimens: Clinical Trial U. M. MORGAN, L. PALLANT,B. W. DWYER,D. A. FORBES, G. RICH, AND R. C. A. THOMPSON
- The Prevalence of Cryptosporidium Infection in Neonatal Diarrhoeic She ep Lambs with Observation of Resolution using Paromomycin. Osman A Hameed,Taj Elsir SA Abu-Zeid,Ghulam Rasool,Albadri Makki,Mohamed Khidr Taha and Brigitte Duquesne
- *1 Comparison of diagnostic sensitivity and specificity of seven Cryptosporidium assays used in the UK Free Rachel M. Chalmers, Brian M. Campbell, Nigel Crouch, André Charlett, Angharad P. Davies,
- *3 Zoetis- Veterinary Diagnostic Laboratory, University of Minnesota, St. Paul, Minnesota.
- *4 BioNote Clinical Evaluation: Anigen Rapid Rota Ag Test Kit Diagnostic,Sensitivity and Specificity, Zoetis LLC.
- Feeding Activated Charcoal from Bark Containing Wood Vinegar Liquid (Nekka-Rich) Is Effective as Treatment for Cryptosporidiosis in Calves S. Watarai,*1 Tana,† and M. Koiwa‡
- Fritz Rexrodt SWAVET RSA PTY Ltd- Afrisan
- Stephan Durand -Aqu Viventum, Belville SA